You'll never be constipated again in your life after reading this
Complete Holistic and Functional Constipation Protocol
If you experience these;
Infrequent bowel movements less than 3 times per week
Hard, dry, or lumpy stools
Straining during bowel movements, feeling like you need to push to pass stool
Feeling of incomplete evacuation
Fullness, tightness, or cramping in the belly
Sensation of blockage like there’s an obstruction preventing stool passage
Needing assistance to pass stool, using hands to press on the abdomen
Passing only small amounts at a time
Smelly flatulence
This is for you!
First we will discuss causes of constipation (this section is important for people who do not know what’s causing them to become constipated).
Next, what stool forms reveal about our gut health. It includes what gut markers are important to consider for constipation. This section will interest individuals who have done GI-stool testing previously or Practitioners who want to understand functional markers for gut and constipation.
Next will be the Don’ts of constipation.
Finally there will be a constipation protocol, how I treat constipation from multiple angles using different tools at disposal.
Causes of constipation
Your are not eating enough food or chronically under eating
90% of people suffering from constipation do not know this fact! When you’re eating infrequently there won’t be enough food to create large enough stool that are enough to be propelled through the colon. Not eating enough will induce constipation;
1. There’s not enough bulk to form stools. Feces is made up of the waste products of your food, less food = less stool to pass.
2. There’s not enough energy for smooth muscle contraction aka peristalsis making it harder to move the waste from your intestines. This overall slowing of muscle contraction in the gut leads to constipation.
You think I have oversimplified it? Keep on reading and you’ll find your answer!
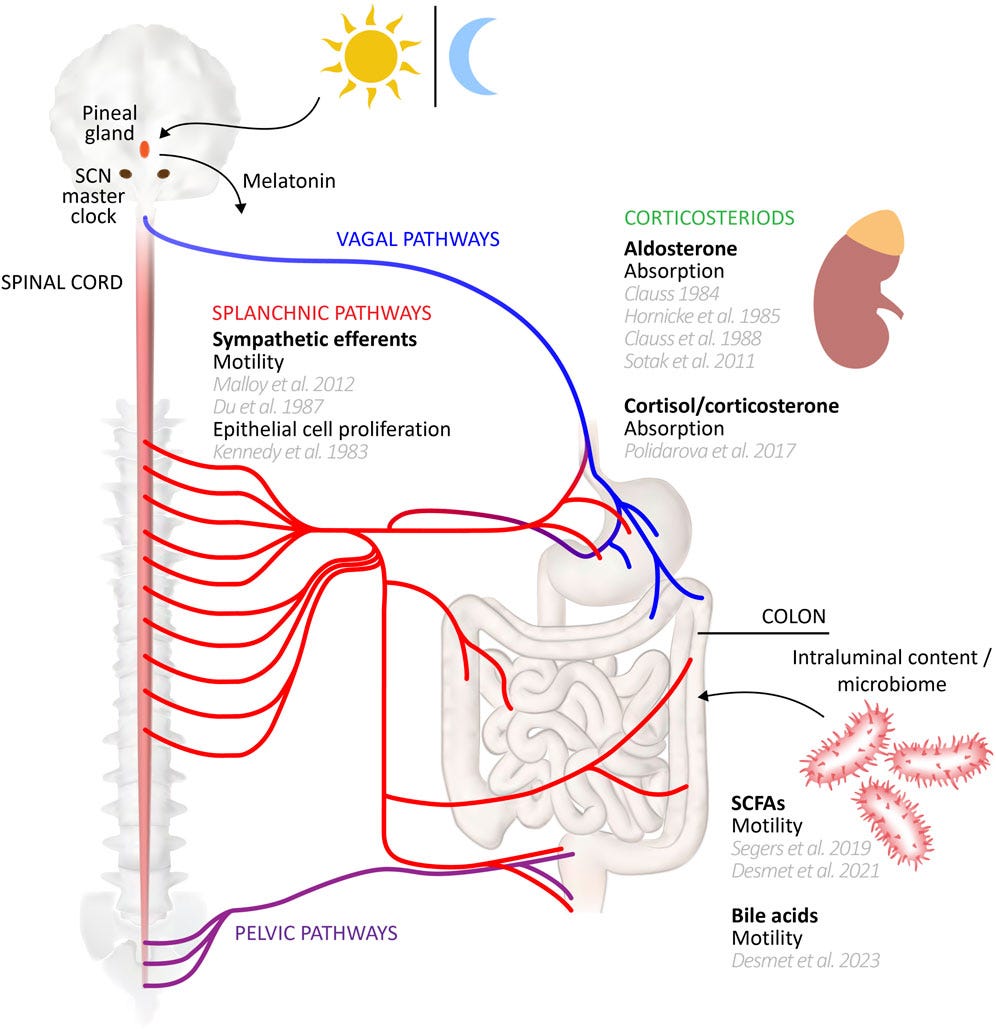
Messed up circadian rhythm
Everything inside your body, each cell, each microbiome has its own circadian rhythm. By definition a circadian rhythm is your body’s internal 24-hour clock, regulated by the suprachiasmatic nucleus (SCN) in the brain, that controls cycles of sleepiness and alertness, hormone production, body temperature, and other physiological processes which receive signals from the sun. Your gut microbiome has its own circadian rhythm. Gut motility, microbiome, hormones, enzymes and colonic function depends on circadian inputs.
For example, irregular sleep patterns can confuse the internal body’s peripheral clocks. Poor sleep imbalances melatonin and cortisol hormones and gut microbiotia. There’s much research now using melatonin as a beneficial supplemental tool for inflammatory bowel diseases. Sleep deprivation can alter gut micro-biotic balance which can progress to gut dysbiosis, constipation and IBS. Defection and need to defecate is an indication of colonic motility showing daily rhythmicity peaking in active periods of the day. Not only that, circadian inputs help modulate your gut microbiome that’s necessary for the production of short chain fatty acids in your gut. The microbes in the gut, especially in the large intestine, ferment dietary fibers and resistant starches that the body cannot digest. This process produces beneficial metabolites, including SCFAs like acetate, propionate, and butyrate. Not only does the body clock modulate the microbiome, but the SCFAs produced by gut bacteria can also influence the host’s circadian rhythms.
Low potassium & Magnesium = poor hydration
Lets not forget that potassium is an electrolyte vital for the proper functioning of smooth muscles, including those in your intestines. Potassium is a vital ingredient for stomach acid production as well. When potassium levels are low, the involuntary muscle contractions that move food and waste through the digestive tract can become impaired, leading to constipation. Potassium is critical for nerve potential as it is key to establishing and maintaining the neuron’s resting membrane potential and voltage-gated potassium channels in your cell membranes. Potassium also helps maintain membrane potential via sodium-potassium-pumps. These pumps are crucial for maintaining intestinal fluid balance and muscle function, and its disruption can contribute to constipation. A low dietary intake of potassium, which impairs the pump, can slow intestinal motility and lead to constipation. Recommended adult dosage per day: Potassium: 3,200 mg/day.
Magnesium citrate is called an osmotic laxative that is occasionally used to treat constipation. Why? Because magnesium can draw water into the intestines to soften and bulk the stool, which helps relieve occasional constipation. There are various forms of magnesium and use depends on what you are trying to achieve from it. Just like potassium, magnesium is vital for the intestines to function properly because it regulates muscle contractions for normal bowel movements, increases water in the colon to soften stools, and acts as a cofactor for digestive enzymes essential for breaking down food. As I’ve mentioned, the type of magnesium you may want to use depends on what reason you are using it for. Recommended adult dosage per day: Magnesium: 350 mg/day.
Poor bile flow / liver issues
Poor bile flow and poor bile quality (thick and stagnant bile) is also important to consider if you are noticing unusual changes in your bowels. Poor bile flow aka cholestasis can cause constipation because undigested fat slows down intestinal motility. Symptoms of poor bile flow include light-colored or foul-smelling stools, nausea, and bloating. It can stem from liver disease, bile duct obstructions like gallstones, or gallbladder issues, all of which hinder bile from reaching the intestines.
Bile salt malabsorption should also be considered. Bile in the intestine helps digest fats, neutralizes stomach acid, and has antimicrobial effects, but high concentrations can cause diarrhea, affect gut health and you should be on a look out if you are experiencing any changes in your stools. Bile also influences intestinal secretion, motility, and absorption of minerals like iron and calcium, while also promoting the growth of beneficial gut bacteria and suppressing harmful ones.
Bile is absolutely critical for gut health and constipation because bile is your “toxin-taxi”. Bile is how your liver transports conjugated and neutralized toxins (like mycotoxins, heavy metals, hormones (like estrogen), thyroid hormone metabolism, prevent pathogens overgrowth, cholesterol, xenobiotics and other drugs, supplements and environmental pollutants. In short all lipophilic, fat soluble substances (good or bad) leave the liver via bile to the gut and make their way out in stools. If you are having trouble with poor bile flow, read this bile blueprint that gives step-by-step guide and functional tools to improve bile flow!
Physical activity
Movement is still an OG relief for constipation. Physical activity improves constipation by stimulating gastrointestinal motility, decreasing transit time, moving entrapped gases in the gut and strengthening the abdominal muscles necessary for defecation. If you are not moving your body, things will get stagnant inside your body, blood, lymphatic system, and the gut. This stagnation will breed diseases like constipation, bloating, IBS, indigestion and GERD.
This analysis of 13 studies with 119 426 participants and 63 713 cases showed higher levels of movement of all kinds, were associated with a decreased risk of constipation. “Our comprehensive analysis showed that a moderate-to-high PA level acted as a protective factor against constipation, significantly reducing the overall constipation risk. This supports an inverse relationship between PA and constipation.”
Physical activity protects you not just from constipation, it includes gastrointestinal diseases like; IBS, IBD, and colorectal cancer.
Physical Exercise as a Therapeutic Approach in Gastrointestinal Diseases
Low fiber because you’ve been trying carnivore
With a carnivore diet fiber gets important. A lot of people might argue that fiber is not important for humans. The thing is people who refute fiber being important for gut health have absolutely no idea about fiber’s types. Dietary fiber especially prebiotics! Fiber is a type of carbohydrate → soluble and insoluble → comes from the plants precisely their cell walls. “Fibers cannot be digested by the human gut” that’s the whole point! Soluble fiber reaches the gut and dissolves into water to form a gel-like substance that gets fermented by bacteria and gets broken down into short chain fatty acids (SCFAs), which can be used by colon cells as energy and other by being indigestible, it stays in our gut longer helping us form the stool bulk. When we eat fibers we are controlling the absorption and uptake of carbs from the gut to enter circulation a little late and help us delay the blood glucose surge, absorb and transform secondary bile, produce beneficial fatty acids, promote bacterial diversity and absorb and remove toxins via stools.
The overconsumption of fibers is where people go wrong. Yes, pants are full of oxalates, lecithins, goitrogens, phytoestrogens, phytates, and tannins that can prevent nutrient absorption in gut and cause deficiencies (like zinc, calcium, vitamin D, iron and magnesium). You may not need them for proper development (and this is why toddlers and children can skip vegetables) but you adults can find fibers (prebiotics) extremely beneficial. More is not always better. If you have serious gut imbalances like dysbiosis and SIBO, inflammatory conditions like IBS and IBD you can exacerbate the problem with too much fibers. If you have these conditions, become strategic with fiber intake; seasonal fruits, organic potatoes, use cooked vegetables only such as making stews and broths and then introduce probiotics and prebiotics. 28-30g fiber daily is recommended but this amount usually depends on individual’s needs and tolerance.
Nutritional deficiencies
We have already covered potassium and magnesium. Now we will discuss other nutrients like vitamin C, zinc, B12, thiamine, choline, and low fat diets.
Zinc: zinc has many roles in our digestive system. Zinc is essential for stomach acid production, maintaining the integrity of tight junctions, which regulate the permeability of epithelial barriers, including the gut and the blood-brain barrier. In zinc deficiency our intestinal barrier falls apart and negatively impacts the absorption of water and electrolytes in the gastrointestinal tract. Zinc deficiency can lead to gut microbiome shifts and inflammation. All of these will lead to constipation and leaky gut, combination of this will bring havoc on your health - constipation will keep waste in your gut for longer periods of time and a leaky gut will reintroduce the waste and toxins that must be eliminated. Recommended dosage for zinc is 30 mg/day, it highly depends on your condition, specific needs and goals, plus I recommend you get it from food sources, supplementation may disturb the balance between copper and zinc.
Vitamin C: this vitamin has in human health overall. Digestive system specific roles are; enhance iron absorption, strengthen the gut barrier through collagen production, modulate the gut microbiome, and act as a potent antioxidant to protect against inflammation and oxidative stress in the digestive tract. Vitamin C also helps inhibit the pathogenic overgrowth like Helicobacter pylori bacteria and histamine overload. The remaining amount of vitamin C that is not actively absorbed osmotically in your gastrointestinal tract, draws water into the intestines and softening stools. Recommended dosage for zinc is 600mg per day taken entirely from natural food sources! Supplementation is recommended under supervision and short-term as high dose vitamin C causes kidney stones.
B12: vitamin B12 only gets absorbed in your gut. It is essential for nutrient absorption because it’s a cofactor in critical enzymatic reactions that support overall gut health, gut motility, DNA synthesis, the creation of red blood cells and function of the autonomic nervous system. Homocysteine and nitric oxide is neutralized by B12 and protects cells from nitrogen oxygen species. Low stomach acid will mean low B12 and combined with low gut absorption and motility will lead to constipation. Vitamin B12 does not come from plant sources so you will need to eat more animal products. The highest source of B12 is beef liver, but obviously do not eat the entire liver in one day.
Thiamine: you know thiamine (Vitamin B1) is essential for nervous system health as it provides energy for brain cells by converting carbohydrates into energy, supports the transmission of nerve signals, helps maintain myelin sheath integrity, and is involved in the synthesis and function of important neurotransmitters, all of which are vital for proper brain and nerve function, including muscle contraction and nerve regeneration. Thiamine has critical roles in digestive track → a vital cofactor for enzymes involved in energy production through carbohydrate and amino acid metabolism, helps maintain gut motility and integrity, and influences neurotransmitter activity to support normal bowel function. B1 is also involved in the synthesis of acetylcholine, a neurotransmitter that plays a role in gut muscle contraction. Thiamine possesses antioxidant properties, protecting the gut from damage and inflammation, all of which are important to consider if you are experiencing chronic constipation! Dosage starts anywhere from 100mg to 400mg (depending on your situation and need), 1x daily for two weeks. It is important that you consume thiamine from food sources because we should not supplement it for longer periods of time.
Choline: Choline is a vitamin like nutrient essential to the digestive system primarily through its crucial role in fat metabolism, liver function, and communication within the gut. Choline is one of many ways your gut and brain axis is linked. Choline is a precursor for acetylcholine, a neurotransmitter to stimulate the smooth muscles of the intestines, increase contractions that push food along the digestive tract. Deficiency of choline makes you prone to constipation. Acetylcholine also triggers the release of digestive juices, such as salivary and gastric secretions, which aid in breaking down food. Choline is not just important for brain development but it’s critical for our overall digestive health. Now learn this with me and never forget it again! Choline bound to phospholipids is absorbed more effectively. Choline in eggs is in the form of phosphatidylcholine (which is a part of cell membranes and a component of your bile!). So, one egg yolk gives you 115 mg per serving and 4 egg yolks will provide approx. 460 mg choline. RDA of choline for adult men is 550 mg/day and adult women is 425 mg/day that approx. Pregnant and lactating women need 450-550 mg/day, fulfilling your needs.
Low-fat diets: fat and lipids are the lubricants of your body. On the outside, fats provide your skin with oils it needs to keep skin hydrating and soft. On the inside, fats and oils provide lubrication in your intestines that makes them slippery to propel bowels and makes stool soft. Dietary fats help stool retain some water, contributing to a softer consistency. Sources of these fats and oils matter for you. We will discuss this in the following protocol.
Underlying conditions (pathogens overgrowth, undiagnosed celiac disease)
If you have chronic constipation and other bowel issues but you do not know why it’s happening, it could be dysbiosis, small intestinal bacterial overgrowth (SIBO), and celiac disease can lead to constipation. Some species of bacteria and archaea, particularly Methanobrevibacter smithii, produce methane as a byproduct and slow down intestinal transit time, resulting in constipation. Any kind of imbalance can decrease the population of beneficial bacteria like coprococcus, ruminiclostridium, and bifidobacteria, which produce SCFAs. These fatty acids help regulate gut motility and promote regular bowel movements. The resulting unhealthy microbiome can weaken the intestinal lining, causing low-grade inflammation impacting the enteric nervous system (the “second brain” in the gut) and slow down intestinal movement. Gut bacteria are key regulators of serotonin, a neurotransmitter that plays a major role in intestinal contractions and motility and can interfere with this signaling, leading to slower transit.
Celiac disease is often associated with diarrhea, it can also cause chronic constipation in some people, affecting both children and adults. When a person with celiac disease eats gluten, their immune system attacks the small intestine, damaging the tiny, finger-like projections called villi and the result will be malabsorption causing the stool to become dehydrated and hardened, leading to constipation instead of diarrhea. The chronic inflammation caused by celiac disease can potentially affect the nerves in the gut, which also slows down intestinal motility.
Undiagnosed thyroid issues
Thyroid hormones control your metabolism and ability to regulate body temperature. They also regulate many bodily processes, including gastrointestinal motility. If your thyroid is slow obviously your body does not have enough energy to maintain peristalsis, leading to slower transit time. This allows the colon to reabsorb more water from the stool, causing it to become hard, dry, and difficult to pass. Low or insufficient thyroid hormone levels can decrease the contractility of the smooth muscles in the gastrointestinal tract contributing to a sluggish digestive system. Hypothyroidism can lead to lower production of stomach acid (hypochlorhydria), which is essential for proper digestion and nutrient absorption. Incomplete digestion can affect bowel function and contribute to discomfort. They can also disrupt the natural balance of gut bacteria, contributing to bloating, gas, and irregular bowel movements. Hypothyroidism can coexist with or trigger other gastrointestinal issues that also cause constipation, such as SIBO and IBS.
Stress and anxiety
Emotions have a greater impact on our digestive system more than many of us anticipate. Stress and anxiety have the ability to affect the gut-brain axis and cause constipation by triggering a “fight-or-flight response” that diverts blood from the digestive system, slowing intestinal movements. During this response, hormones like epinephrine and cortisol are released, which can disrupt the gut-brain axis, reduce motility, affect the gut microbiome, and slow the passage of waste through the digestive tract, leading to constipation. Stress can alter serotonin levels and increase intestinal permeability, further disrupting digestive function. Melatonin has a relaxing effect on our intestines. Under normal conditions, melatonin is dominant at night and bowel movements at night are one of many signs of circadian misalignment. When we are approaching the day, cortisol naturally rises and we get the urge to empty our bowels in the morning. But this response is altered under chronic conditions of stress. Chronically elevated cortisol can cause the colon to spasm or alter intestinal movement, potentially leading to constipation or cramps.
Medications
Many of you do not know this but the medications or any new supplement you introduced lately could be causing your constipation. Many over-the-counter medications cause constipation and change in stool consistency. Medications may draw water from intestines, cause dehydration and harden the stool, may slow down digestion and gut motility. Few examples;
Iron supplements – anemia; pull water from stool → dry, slow passage
Calcium carbonate – bone/heart health → dry stool by altering fluid in the intestine
Vitamin D – bone health; raises calcium levels → constipation
Fiber supplements – constipation support; may absorb too much water → hard stools
Berberine → high doses may cause constipation
Opioids – pain relief → slow bowel movement.
Psychiatric meds → strongly constipating
Antidepressants – depression/anxiety → reduce gut motility
Blood pressure meds – hypertension → reduce bowel activity
Antihistamines – allergies→ relax gut muscles
Antacids – heartburn→ harden stool
Poor dietary habits (highly processed foods, concentrated fructose foods etc)
Do not underestimate the processed snack you might be having. Highly processed foods are not real foods. They are packed with foreign substances that are not beneficial for our gut. Preservatives and antimicrobials such as sulphites, sulphur dioxide, anti-fungal agents, disinfectants, fumigants, antibiotics, and related compounds can disturb the gut microbiota and irritate the intestinal lining. Color and appearance agents like dyes, artificial colours, bleaches may further disrupt microbial balance and place stress on detoxification pathways. Texture and stability agents including emulsifiers, thickeners, stabilisers, texturises, anti-foaming, and anti-caking agents can thin the protective mucus layer of the gut and promote inflammation. Sweeteners and taste modifiers such as artificial sweeteners, neutralisers, and alkalizers may alter microbial composition and slow bowel function. Processing and shelf-life agents like humectants, drying agents, gases, hydrogenators, hydrolysers, maturers, and even steroids can interfere with digestion and absorption, collectively contributing to constipation and broader gastrointestinal issues. Highly processed foods promote constipation by stripping out fiber, which normally adds bulk and water to stool.
Physically abnormalities (rectal prolapse, anal fissures)
Physical abnormalities like rectal prolapse and anal fissures can cause constipation by creating a painful and obstructive cycle that prevents normal bowel movements. Presence of an anal fissure often caused by passing hard or large stools. Rectal prolapse also contributes to constipation. Any kind of intestinal obstruction can also lead to chronic constipation that gets worse without immediate emergency treatment.
Hormonal fluctuations during your natural menstrual cycle (progesterone)
Luteal phase constipation is progesterone by acting as a natural muscle relaxant including the muscles in intestine. This relaxation effect slows the movement of food and waste through the digestive tract by reducing contractions in the gut lining. The slower transit time allows more water to be absorbed from the stool, leading to harder bowel movements that last for two days or more. Other hormones like estrogen can inhibit the smooth muscle contractions of the colon, which are necessary for moving stool through the digestive tract. This impaired contractility slows down bowel movements and causes constipation. Infrequent bowel movements during the second half of your cycle (luteal phase) can be specifically due to progesterone rising but the persistent constipation that happens in estrogen dominance throughout the cycle could be estrogen at play.
Pregnancy
Continuing the previous point, pregnancy is marked by increased progesterone levels (because progesterone is a pro-fertility hormone, it is the reason why endometrial lining is sustained to keep pregnancy miscarriage free). Pregnancy constipation is caused by increased progesterone levels and growing uterus, which puts pressure on the bowels. It can also be worsened by high iron intake from prenatal vitamins. To relieve it, pregnant women should pay close attention to their sleep wake cycle, rest, hydration, their meals, take cooked vegetables stews and broths, get regular light exercise like walking, and not delay bowel movements. Physical movement is extremely important during pregnancy to avoid constipation!
What stool form reveal about my gut
Now we have understood the causes of constipation. Next we will dive into what’s happening in your gut based on the type of stools you might be having.
I’ve used a Bristol stool chart to make the stool reference but this chart is not like the regular chart you may see on social media. To help you understand the nuance beyond surface level stuff I will be teaching you the what might be happening inside your intestines based on stool forms, updated with bacterial metabolism, GI-MAP Microbial Insights, GI-MAP Intestinal Markers and come with clinical notes details so you understand it clearly. Bristol stool chart is a noninvasive, less expensive way to interpret someone’s gut functioning to limited extents.
If you are not a practitioner it might be a little hard for you to decode. Read the following notes to understand it better. Every stool type is tied to:
Transit speed (how long stool stays in the gut)
Bacterial balance (beneficial, opportunistic, or pathogenic)
Bristol Stool Scale Explained - Gut Bacteria, Markers & Meaning
Types 1-2: Hard, Lumpy Stool (Constipation)
When stool is hard and lumpy, it means that transit through the colon is very slow. The longer stool sits, the more water is reabsorbed, leaving it dry and compact. This slow movement allows certain microbes to thrive. For example, Methanobrevibacter, a methane-producing microorganism, becomes abundant. Constipated people often have smelly flatulence, highlighting gas buildup. Methane slows down gut motility even further, reinforcing the cycle of constipation. Akkermansia, a bacterium that feeds on the gut’s protective mucus layer, can also increase in this low-water, slow-transit environment.
The GI-MAP tests of these patients show that people with constipation often have higher levels of Enterococcus, Bacillus, and Methanobacteriaceae, which are opportunistic organisms that can disrupt balance if overgrown. Bacteroides fragilis, another common gut bacterium, may also rise in this pattern. Key stool marker here is β-glucuronidase, an enzyme produced by Bacteroides, Clostridia, and E. coli. When elevated, it “reactivates” estrogens in the gut that should have been excreted, pushing them back into circulation. This can lead to hormonal imbalances such as estrogen dominance. Men and women both should pay attention to this specifically.
Clinically, this stool type reflects a constipation phenotype. Symptoms often include bloating, IBS-C (constipation-predominant irritable bowel syndrome), and discomfort. Over the long term, slow transit alters bile acid metabolism and prolongs toxin exposure, which can raise the risk of gallstones and bowel cancer.
Types 3-4: Smooth, Soft Stool (Healthy/Normal)
This stool form is considered healthy because transit is balanced, not too fast, not too slow. When stool passes at the right pace, the gut microbiome can maintain its richest diversity. Beneficial bacteria flourish, including Faecalibacterium prausnitzii and Roseburia, both of which are major producers of butyrate, a short-chain fatty acid (SCFA). Butyrate nourishes the cells lining the colon and helps control inflammation. Other helpful microbes, such as Bifidobacterium and Lactobacillus, also thrive here, supporting digestion, immune balance, and the maintenance of a healthy gut pH.
Clinically, this stool type indicates a protective gut environment. The microbiota are diverse and stable, the mucosal barrier is strong, and inflammation is kept in check. People with this stool pattern generally have better resilience against infections, food sensitivities, and inflammatory conditions.
Type 5: Soft Blobs (Borderline Loose)
When stool appears as soft blobs with clear edges, it signals that transit is slightly faster than normal. This shortens the time available for bacteria to ferment dietary fibers. Under these conditions, species like Bacteroides gain an advantage, since they grow quickly and can thrive with shorter transit. If the immune barrier is not functioning optimally, opportunistic microbes such as Streptococcus and Staphylococcus may begin to overgrow.
The key marker here is SIgA (secretory immunoglobulin A), the gut’s first line of immune defense, is usually normal, reflecting a well-regulated immune barrier. If SIgA is low or fluctuating, the immune system’s ability to control opportunists is weakened. This can set the stage for dysbiosis, where less beneficial bacteria start to outcompete healthier ones.
Clinically, this pattern may represent an early diarrhea phenotype. It is not necessarily abnormal but can point to mild malabsorption or the beginnings of microbial imbalance. If persistent, it may progress toward more significant digestive issues.
Types 6-7: Mushy or Watery Stool (Diarrhea)
Loose or watery stool indicates very rapid transit. Food and waste move through the gut so quickly that there is little time for nutrient absorption or bacterial fermentation. As a result, microbial richness declines, and fast-growing bacteria such as Bacteroides and Prevotella dominate. The rapid movement also lowers stool pH, creating a more acidic colonic environment.
The GI-MAP tests show that this stool type often accompanies an overgrowth of opportunistic or pathogenic microbes, including Klebsiella, Proteus, Pseudomonas, Salmonella, Giardia, and Norovirus. These organisms can drive or worsen diarrhea. Several stool markers are important here. Steatocrit levels are often high, reflecting fat malabsorption, fats are being lost in the stool instead of absorbed. Pancreatic elastase-1 (marker of digestive enzyme output) may be low, showing that the pancreas is not adequately breaking down food. SIgA is typically high in acute infections as the immune system fights off pathogens, but in chronic diarrhea it may be low, signaling immune exhaustion.
Clinically, this stool type reflects an infectious or inflammatory diarrhea phenotype. It often comes with urgency, nutrient malabsorption, and microbiome instability. Beneficial species are diminished, while harmful or fast-growing organisms take over and progress to something concerning.
Transit time simple at-home test
Apart from these functional tests I use a holistic remedial method to check my clients or patients transit time. Another simple and non-invasive way to measure how long food takes to travel through the digestive system, from mouth to stool is the “corn test”. The test works because the outer shell of sweetcorn kernels is made of cellulose. It is a fiber humans cannot fully digest and the yellow corn hulls pass through the digestive tract unchanged. By checking how long it takes for the first kernels to appear in the stool, and how long until the last kernels are seen, we can estimate their gastrointestinal transit time. But the only downside is you will have to check your stools each time :) in the toilet.
There’s a study done on corn test where health science students in Namibia ate 75 grams of whole-kernel sweetcorn. They were asked to record the exact time of eating, the time they first saw corn in their stool, and the time they last saw corn. What it shows:
If corn shows up quickly (less than a day), it suggests fast transit → food is moving rapidly through your gut.
If it takes much longer (2-3 days or more), it suggests slow transit → stool sits longer in the bowel, often linked to constipation.
The corn test demonstrates that “normal” varies widely between people, but it’s a simple, visible marker of how fast or slow your digestion is working. Must remember to swallow the corn kernels whole like a tablet, do not chew them so they can pass through intestines and come out as whole in stools for you to easily identify them.
Don'ts - You really shouldn’t rely on coffee enemas
You really shouldn’t be relying on stool softeners, nicotine, caffeine or coffee enemas to empty your bowels. These are just stimulants, not real solutions, and should not be used long term.
Coffee enemas are extremely dangerous. They might be doing more harm than good for constipation. Coffee enemas depletes your essential minerals, the very electrolytes, your intestines need to propel stool forward. Frequent coffee enemas can delete minerals most people fail to get regularly. Electrolytes are your daily need, you replete them daily because you’re losing them constantly. Regular enemas can cause severe electrolytes imbalances which can result in death. The detoxification claims associated with coffee enemas lack scientific evidence.
Frequent enemas remove potassium, magnesium, sodium, chloride and water. There are some studies that show that coffee enemas upregulate glutathione and dilate biliary ducts but doing coffee enemas randomly without caring for your minerals may be a serious health mistake. Under medical supervision, only done by medical professionals when needed.
First get enough of these, then think about getting an enema;
Sodium: 1,500 mg/day
Potassium: 3,200 mg/day
Magnesium: 350 mg/day
8-9 glasses of water + structured water intake
Now we have set the stage for The Nutrition Protocol for Constipation!
The Complete Holistic and Functional Constipation Protocol is released in my my Private Community, click here to continue reading.





This is really detailed and comprehensive, thank you! As a chronic constipation sufferer, this is massively helpful. ❤️
amazing article! Yes to all these!! 👏🏻